TeleHealth
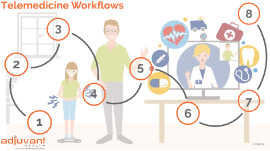
Transcript: Today, incentives are offered to healthcare facilities that implement new technologies; mostly used for electronic systems In coming years, this is expected to change Will be an expectation that organizations are up-to-date Reimbursement will no longer apply to telehealth services This is a trend, so it cannot be know that this will be implemented Increased Use Forecast By: Amy Whitelaw, Alyssa Lyons and Ben Lescault The STARPAHC Project and the Papago Reservation Ultimately, STARPAHC would provide a full communications between the central station on the Papago Reservation, and a fixed satellite clinic at Santa Rosa, a regularly scheduled mobile health clinic, and a full facility hospital-based clinic at Phoenix. Change in Reimbursement Models Telemedicine: the delivery of clinical care via telecommunications technology-diagnosing, treating or follow up with a patient at a distance Examples of Telemedicine A mobile app that lets physicians treat their patients remotely via video-chat A software solution that lets primary care providers send patient photos of a rash or mole to a dermatologist at another location for quick diagnosis TeleHealth vs. TeleMedicine NASA’s influence on telehealth began with the need to track astronauts biomedical responses including HR, oxygen consumption, heat production and and CO2 levels while under extreme conditions Medical personnel at the Mission Control Center at Johnson Space Center (JSC) in Houston would conduct daily medical conferences to review the astronauts health and adaption to zero gravity NASA continues to promote and develop new technologies to advance the practice and safety of their astronauts through biotelemetry Included a control system on the reservation staffed by physicians connected to a remote clinic and also a mobile health unit Telehealth: the use of telecommunications technologies to deliver health-related services and information that support patient care, administrative activities and health education Examples of Telehealth: A public health app that alerts the public of a disease outbreak A video-conferencing platform for medical education What TeleMedicine Looks Like TeleHealth & TeleMedicine MHealth (Mobile Health) Implementation: “The practice of medicine and public health supported by mobile devices” Smartphones Tablets Other Devices Increase number of users and increase user depth Patient security is important, as more information will be accessed Patient responsibility is required while using mHealth systems Records cannot be shared with outside members; HIPAA violation Abdelhak, M., & Hanken, M. (2016). Health Information (5th ed., Vol. 1). St. Louis, MO: Elsevier. Future of Telemedicine and Telehealth - eVisit Telehealth Solution. (n.d.). Retrieved April 16, 2016, from http://evisit.com/future-of-telemedicine-7-trends-shaping-the-future-of- telehealth/ Medscape Log In. (n.d.). Retrieved April 16, 2016, from http://www.medscape.com/viewarticle/840335 M. (2014, May 24). Telehealth: When technology meets health care. Retrieved April 14, 2016, from http://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878 Benefits of Telehealth / Telemedicine? (n.d.). Retrieved from http://www.setrc.us/index.php/what-is-telehealth/benefits-of-telehealth-telemedicine/ Josh Savitz RCL Blog. (n.d.). Retrieved from http://sites.psu.edu/savitzrclblog/ Telehealth Start-Up and Resource Guide. (2014, October). Retrieved April 15, 2016, from https://www.healthit.gov/sites/default/files/telehealthguide_final_0.pdf Telemedicine Guide. (2016, January). Retrieved April 15, 2016, from http://evisit.com/what-is-telemedicine/ What is Telemedicine? (2012, January). Retrieved April 15, 2016, from http://www.americantelemed.org/about-telemedicine/what-is-telemedicine#.VxGaK2OUldp Freiburger, G., Holcomb, M., & Piper, D. (2007). The STARPAHC collection: Part of an archive of the history of telemedicine. J Telemed Telecare Journal of Telemedicine and Telecare, 13(5), 221-223. doi:10.1258/135763307781458949 Thompson, V., Decker, B., Hardash, J. A., & Summers, R. O. (2012). NASA (In)novation Ecosystem: Taking technology innovation from buzz to reality. 2012 IEEE Aerospace Conference. doi:10.1109/aero.2012.6187447 Increases access to care Improves health outcomes Improves quality of care Improves timeliness of care Reduces healthcare and cost Improves patient safety Assits with healthcare professional shortages Supports clinical educational programs Promoting Patient Care by Communication The technology used included: Two way video Audio and data communications Home Health Monitoring Phsyicians use the help of machines that are used by the patient in their home Commonly used with diabetes and hypertension patient The Start of TeleHealth Teleradiology System: In the 1950’s major university-based medical hospitals began to put telemedicine into practice by transmitting radiologic images via telephone including X-rays, CT’s and MRI’s The University of